Dilated cardiomyopathy (DCM) is a condition where your heart’s left ventricle enlarges and weakens, making it harder to pump blood effectively. It can result from genetic factors, infections, alcohol use, or exposure to toxins. As your heart structural changes, you might notice symptoms like fatigue, shortness of breath, or swelling. Understanding how DCM impacts your heart and exploring available treatments can help you manage the condition better—more details are just ahead.
Key Takeaways
- Dilated Cardiomyopathy (DCM) involves enlargement and weakening of the heart’s left ventricle, reducing its ability to pump blood effectively.
- Causes include genetic mutations, viral infections, excessive alcohol intake, certain drugs, and environmental toxins.
- Symptoms often include fatigue, shortness of breath, swelling in legs or abdomen, which may develop gradually.
- Diagnosis primarily relies on echocardiogram and cardiac MRI to assess heart structure, function, and tissue damage.
- Treatment involves medications, lifestyle changes, and possibly surgical interventions to manage symptoms and prevent complications.
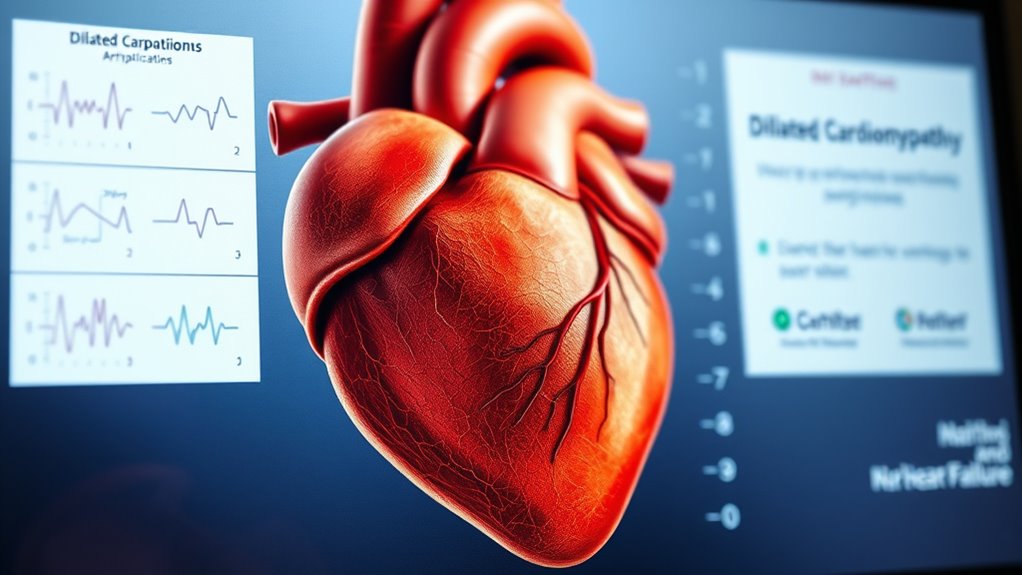
What Is Dilated Cardiomyopathy?
Dilated cardiomyopathy is a condition where the heart’s main pumping chamber, the left ventricle, becomes enlarged and weakened. This weakening reduces the heart’s ability to pump blood effectively, leading to symptoms like fatigue and shortness of breath. Genetic factors can play a significant role, as some people inherit traits that make their heart more susceptible to dilation. Lifestyle influences also matter; excessive alcohol consumption, poor nutrition, or unmanaged stress can contribute to weakening the heart muscle over time. While the exact cause isn’t always clear, understanding these factors helps you recognize how both inherited traits and daily habits influence your heart health. Addressing lifestyle influences and knowing your family history can be crucial steps in managing or preventing dilated cardiomyopathy. Additionally, ongoing advancements in AI and automation are improving diagnostic tools and treatment options for heart conditions like DCM.
Causes and Risk Factors of DCM
Several factors can increase your risk of developing dilated cardiomyopathy, whether through genetic mutations or lifestyle choices. Genetic mutations may be inherited, making you more prone to DCM. Viral infections, such as myocarditis, can also damage your heart muscle, triggering DCM. Other risk factors include alcohol abuse, certain drugs, and exposure to toxins. Family history is important to contemplate, as DCM can run in families. Understanding these causes helps you identify potential risks early. Here’s a quick overview:
| Cause/Risk Factor | Description |
|---|---|
| Genetic mutations | Inherited gene changes affecting heart muscle genetic predisposition |
| Viral infections | Viral damage leading to inflammation and weakness |
| Alcohol abuse | Excessive drinking weakens heart muscle |
| Drug exposure | Certain medications harm the heart |
| Toxins | Environmental toxins can increase risk |
A better understanding of heart muscle health can contribute to early detection and prevention strategies for DCM. Additionally, ongoing research is exploring genetic testing to identify individuals at higher risk before symptoms develop, emphasizing the importance of genetic screening for at-risk populations.
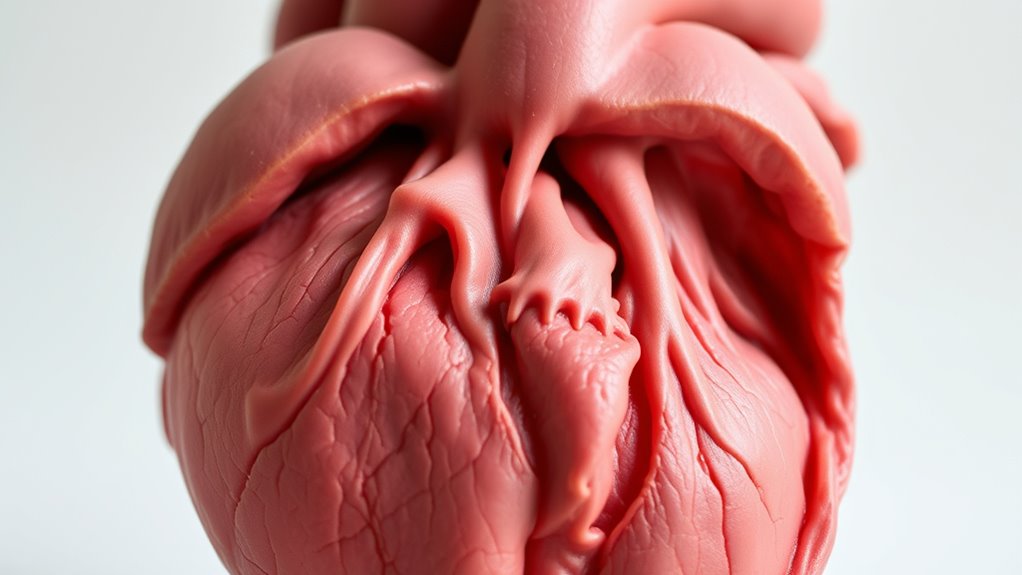
How DCM Affects the Heart’s Structure and Function

With dilated cardiomyopathy, your heart’s chambers become enlarged and weakened, making it harder to pump blood effectively. This structural change reduces the heart’s ability to contract strong enough to meet your body’s needs. As a result, your heart’s overall efficiency in pumping blood drops, leading to symptoms like fatigue and shortness of breath.
Chamber Enlargement and Weakness
As dilated cardiomyopathy progresses, the heart’s chambers become enlarged and weakened, impairing their ability to pump blood effectively. This enlargement stretches the heart muscle, leading to muscle weakness and reduced strength. You might notice these changes through symptoms like fatigue or shortness of breath. Here’s what happens:
- The heart chamber expands, making it harder for your heart to contract efficiently.
- The weakened muscle can’t generate enough force, decreasing blood flow.
- The overall structure becomes less effective, setting the stage for further heart problems.
This combination of chamber enlargement and muscle weakness causes your heart to struggle, compromising its ability to meet your body’s needs. Understanding these changes helps you recognize early signs and seek proper medical care.
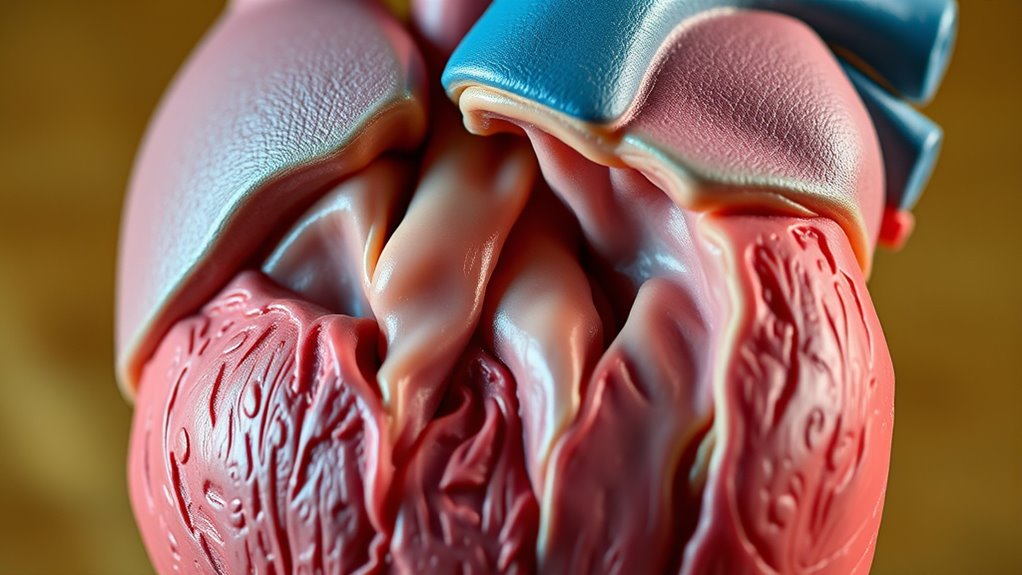
Reduced Pumping Efficiency
When your heart’s chambers enlarge and weaken, its ability to pump blood efficiently declines. This reduced pumping efficiency means your muscles and organs may not get enough oxygen and nutrients, leading to symptoms like fatigue and exercise intolerance. You might find yourself short of breath during daily activities or exertion. Managing DCM often involves medication management to improve heart function and reduce symptoms. Medications like ACE inhibitors or beta-blockers help support your heart’s pumping ability and prevent further deterioration. As the heart’s capacity diminishes, your quality of life can be affected, emphasizing the importance of adhering to treatment plans. Recognizing these signs early allows your healthcare team to tailor therapies that enhance your heart’s efficiency and help you maintain a more active lifestyle. Additionally, understanding how the heart’s structure and function are impacted can aid in early detection and effective management of the condition influencing prognosis. The diagnostic tools used to assess DCM include echocardiography, MRI, and blood tests, which help determine the extent of heart damage and guide treatment options. Being aware of the structural changes in the heart can also facilitate prompt intervention and better outcomes. Moreover, advances in understanding the molecular mechanisms underlying DCM can lead to targeted therapies that improve long-term prognosis.
Recognizing the Symptoms of DCM
How can you identify if you might be experiencing symptoms of dilated cardiomyopathy (DCM)? Recognizing early signs can help you seek treatment promptly. Keep an eye out for:
- Shortness of breath, especially during activity or at rest
- Fatigue that doesn’t improve with rest
- Swelling in your legs, ankles, or abdomen
- Vetted information about the condition can help you understand the importance of early detection.
- Being aware of cardiac function and how it may decline with DCM can empower you to seek timely medical attention.
Your genetic predisposition and lifestyle factors play a role in developing DCM, so if you have a family history or lead a sedentary lifestyle, stay alert. Symptoms may develop gradually, making it easy to overlook them. If you notice any of these signs, consult a healthcare professional to determine if DCM could be the cause. Early recognition increases your chances of managing the condition effectively.
Diagnostic Procedures for DCM

To diagnose DCM, your doctor will typically start with an echocardiogram to assess heart size and function. They might also recommend a cardiac MRI to get detailed images of the heart’s structure. These tests help provide a clear picture of the condition and guide your treatment plan. Ensuring proper diagnosis and understanding of the heart’s condition can be supported by evaluating the effectiveness of air purification in your environment, which can contribute to overall cardiovascular health. Maintaining clean indoor air through HEPA filters can reduce exposure to airborne pollutants that may affect heart health. Additionally, understanding the mechanics of pinball machines highlights how complex systems interact, similar to the intricacies involved in cardiac diagnostics and the importance of proper planning to optimize health outcomes.
Echocardiogram Techniques
Echocardiography stands as the primary non-invasive tool for diagnosing dilated cardiomyopathy (DCM). It uses various echocardiogram techniques and imaging modalities to assess heart structure and function accurately. Here’s what you should know:
- Standard transthoracic echocardiogram (TTE): This common method provides detailed images of your heart’s chambers, wall motion, and ejection fraction.
- Doppler imaging: It evaluates blood flow, helping identify any regurgitation or abnormal flow patterns associated with DCM.
- Contrast echocardiography: When images are unclear, contrast agents improve visualization of cardiac chambers and wall motion.
These imaging modalities help you and your doctor understand the extent of the disease and guide treatment decisions effectively.
Cardiac MRI Insights
Building on the detailed images obtained through echocardiography, cardiac MRI offers a thorough view of the heart’s structure and tissue characteristics in patients with dilated cardiomyopathy. This imaging technique identifies myocardial fibrosis, which can impair heart function and influence treatment decisions. MRI’s high-resolution images reveal scar tissue and help assess the extent of damage. Additionally, cardiac MRI can guide genetic testing by highlighting specific tissue changes associated with inherited forms of DCM. You can use this information to better understand the disease’s progression and tailor your treatment plan. Overall, MRI provides critical insights into myocardial health, making it a valuable tool in diagnosing and managing dilated cardiomyopathy effectively. Moreover, AI-driven diagnostic tools are increasingly being integrated to enhance the accuracy and efficiency of cardiac MRI analysis.
Treatment Options for Managing DCM
Managing dilated cardiomyopathy involves a range of treatment options aimed at improving heart function and reducing symptoms. Your doctor may recommend:
- Medication management: You might take ACE inhibitors, beta-blockers, or diuretics to strengthen your heart and relieve congestion.
- Surgical interventions: In severe cases, procedures like implantable devices or even heart transplantation could be necessary.
- Lifestyle medications: Certain drugs may help prevent blood clots or manage arrhythmias associated with DCM.
These approaches target the underlying issues and help improve quality of life. Your healthcare team will tailor treatments based on your condition severity, aiming to stabilize your heart and prevent progression. Regular monitoring ensures your management plan adapts to your needs.
Lifestyle Changes and Heart Health

Making effective lifestyle changes is essential for supporting your heart health when you have dilated cardiomyopathy. Focus on dietary modifications by reducing salt intake and choosing heart-healthy foods like fruits, vegetables, and whole grains. Managing stress is equally important; practice relaxation techniques such as deep breathing or meditation to lower your blood pressure and reduce strain on your heart. Incorporate regular exercise as recommended by your doctor to strengthen your cardiovascular system. Here’s a quick guide:
| Change | Benefit | Tips |
|---|---|---|
| Dietary modifications | Lower blood pressure, reduce fluid retention | Limit processed foods, avoid excess salt |
| Stress management | Decrease strain on your heart | Practice meditation or yoga |
| Regular exercise | Improve heart function | Consult your healthcare provider before starting new routines |
| Quit smoking | Reduce cardiovascular risk | Seek support programs |
| Limit alcohol | Prevent heart damage | Follow medical advice |
Additionally, avoiding excessive alcohol consumption can help prevent additional stress on your heart. Incorporating heart-healthy habits into your daily routine can further support your recovery and overall well-being. Maintaining proper hydration is also important to support your cardiovascular health. Regularly monitoring your heart health can help detect any changes early and ensure appropriate adjustments to your lifestyle.
Potential Complications of DCM
With dilated cardiomyopathy, you face an increased risk of heart failure, which can weaken your heart’s ability to pump blood effectively. Blood clots may form in your enlarged heart chambers, raising the chance of strokes or other complications. Additionally, abnormal heart rhythms, or arrhythmias, can develop, potentially leading to serious or life-threatening events. Understanding emotional support and seeking appropriate care can help manage these risks effectively. Being aware of local resources can provide additional assistance and guidance during treatment. Incorporating well-being tips such as stress management and emotional resilience strategies can further aid in coping with the emotional challenges associated with DCM.
Heart Failure Risks
Have you ever wondered what happens when dilated cardiomyopathy progresses? It can lead to heart failure, a serious condition where your heart struggles to pump blood effectively. To reduce this risk, consider these key steps:
- Implement diet modifications: Reducing salt intake helps prevent fluid buildup and eases the workload on your heart.
- Manage stress: Chronic stress can worsen symptoms, so find healthy ways to relax and stay calm.
- Monitor symptoms closely: Recognizing early signs like fatigue or shortness of breath allows timely medical intervention, potentially preventing full-blown heart failure.
- Embrace ongoing learning: Staying informed about conditions like angel number soulmate can empower you to make proactive health decisions. Additionally, understanding how spiritual guidance or positive signs might influence your outlook can support overall well-being.
Blood Clot Formation
Blood clot formation is a serious complication that can arise when dilated cardiomyopathy affects your heart’s ability to pump blood effectively. When your heart’s chambers become enlarged and weakened, blood flow slows down, increasing the risk of blood clots forming inside the heart. These blood clots, or thrombus formation, can break loose and travel through your bloodstream, potentially causing blockages elsewhere, like in the brain or lungs. This risk underscores the importance of monitoring your heart health closely. If you develop blood clots, they can lead to serious issues such as stroke or pulmonary embolism. Managing your condition with proper treatment can help reduce the chances of thrombus formation and its dangerous complications.
Arrhythmia Development
When blood clots form inside the heart due to dilated cardiomyopathy, they can disrupt the heart’s electrical signals and lead to abnormal rhythms. These arrhythmias happen because the enlarged, weakened heart muscle affects electrical conduction pathways. You might experience irregular heartbeats, dizziness, or even fainting. Several factors contribute to arrhythmia development:
- Damaged heart tissue creates abnormal electrical pathways, serving as arrhythmia triggers.
- The dilation distorts the heart’s structure, impairing normal electrical conduction.
- Scar tissue from previous damage can interfere with signal transmission, increasing arrhythmia risk.
Understanding these triggers helps you recognize symptoms early and seek treatment. Managing arrhythmias is essential to prevent complications like stroke or sudden cardiac arrest associated with DCM.
Advances in DCM Research and Future Therapies
Recent advances in dilated cardiomyopathy (DCM) research have propelled the development of promising therapies that target the underlying causes and improve patient outcomes. Genetic testing now plays a vital role in identifying inherited forms of DCM, allowing for earlier diagnosis and personalized treatment plans. Researchers are also discovering emerging biomarkers that help detect disease progression and predict patient responses to therapy. These biomarkers, found in blood or tissue, enable clinicians to monitor DCM more precisely and tailor interventions accordingly. Future therapies focus on gene editing, targeted drugs, and regenerative approaches that address the root genetic and molecular factors. These innovations aim to transform DCM management from symptom control to disease modification, offering hope for improved quality of life and long-term survival.
Supporting Patients and Families Facing DCM

Advances in DCM research have opened new possibilities for personalized treatments and better disease management. Facing a DCM diagnosis can be overwhelming, but support is available. Here’s how you can navigate this journey:
Recent DCM advances offer hope through personalized treatments and strong support networks.
- Seek emotional support from mental health professionals or support groups to process your feelings.
- Tap into community resources, such as local clinics or patient organizations that offer education and practical assistance.
- Build a strong support network with family, friends, and healthcare providers who understand your needs.
Frequently Asked Questions
Can Children Develop Dilated Cardiomyopathy?
Yes, children can develop dilated cardiomyopathy. Pediatric diagnosis involves recognizing childhood symptoms like fatigue, shortness of breath, and swelling. If you notice these signs in a child, it is crucial to seek medical help promptly. Early diagnosis allows for better management and treatment, improving their quality of life. Keep an eye on symptoms and consult a healthcare professional if you suspect your child might have this condition.
Is DCM Hereditary or Genetic?
Think of DCM as a family recipe passed down through generations; it can indeed be hereditary. You might want to consider genetic testing if there’s a familial risk, as it helps identify if DCM runs in your family. While not always purely genetic, many cases have a hereditary component, making awareness and early detection vital. So, knowing your family’s health history helps you stay ahead of potential risks.
How Does DCM Impact Quality of Life Long-Term?
Living with DCM can substantially impact your long-term quality of life. You might experience emotional well-being challenges, like anxiety or depression, due to ongoing health concerns. Social adjustment may also become difficult because of physical limitations or the need for regular medical care. However, with proper management, support, and lifestyle adjustments, you can maintain a positive outlook, improve emotional well-being, and adapt socially to lead a fulfilling life despite DCM.
Are There Natural or Alternative Therapies for DCM?
Imagine someone with DCM exploring natural options; they might try herbal supplements like hawthorn, which some believe supports heart health. While lifestyle modifications—such as a balanced diet and gentle exercise—can help manage symptoms, it’s essential to consult your doctor before trying any alternative therapies. Natural remedies may complement conventional treatments but shouldn’t replace prescribed medications. Always seek professional guidance for a safe, effective approach.
What Is the Prognosis for Untreated DCM?
Without treatment, your DCM can worsen over time, leading to severe heart failure or even death. Disease progression speeds up without intervention, making symptoms harder to manage. Treatment outcomes, however, vary; medications and devices can improve quality of life and prolong survival. If you skip treatment, the prognosis worsens markedly, so early diagnosis and management are vital to slow disease progression and improve your chances of a better outcome.
Conclusion
Understanding dilated cardiomyopathy helps you take control of your heart health, much like steering a ship through stormy seas. By recognizing symptoms, making lifestyle changes, and staying informed about new treatments, you can steer toward better outcomes. Remember, you’re not alone—medical advances and support are on your side, guiding you like a lighthouse shining through the darkness. With awareness and care, you can chart a course toward a healthier, stronger heart.